Sofosbuvir
Sovaldi
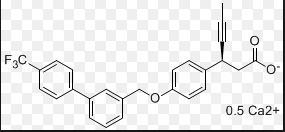
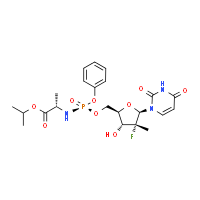
M.Wt: 529.45
Formula: C22H29FN3O9P
Isopropyl (2S)-2-[[[(2R,3R,4R,5R)-5-(2,4-dioxopyrimidin-1-yl)-4-fluoro-3-hydroxy-4-methyl-tetrahydrofuran-2-yl]methoxy-phenoxy-phosphoryl]amino]propanoate
A prodrug of 2′-deoxy-2′-alpha-F-2′-beta-C-methyluridine 5′-monophosphate.
GS-7977, PSI-7977
- GS 7977
- GS-7977
- PSI 7977
- PSI-7977
- Sofosbuvir
- Sovaldi
- UNII-WJ6CA3ZU8B
CAS Registry Number :1190307 -88-0
http://www.ama-assn.org/resources/doc/usan/sofosbuvir.pdf
Indications: Chronic hepatitis C (HCV GT1, GT2, GT3, GT4)
Mechanism: nucleoside NS5B polymerase inhibitor
approved Time: December 6, 2013
,U.S. Patent Number: 7964580,8415322,8334270,7429572;, patent validity: March 26, 2029 (U.S. Patent No.: 7,964,580 and 8,334,270), April 3, 2025 (U.S. Patent No.: 7,429,572 and 8,415,322)
US patent number 7964580, US patent number 8415322, US patent number 8334270,US patent number 7429572 Patent Expiration Date: March 26, 2029 for US patent number 7964580 and 8334270 (2028 in EU); April 3, 2025 for US patent number 7429572 and 8415322
Sales value (estimated): $ 1.9 billion (2014), 6600000000 USD (2016)
Drug Companies: Gilead Sciences, Inc. (Gilead Sciences)
WASHINGTON, Dec. 6, 2013 (AP) — Federal health officials have approved a highly anticipated hepatitis C drug from Gilead Sciences Inc. that is expected to offer a faster, more palatable cure to millions of people infected with the liver-destroying virus.
The Food and Drug Administration said Friday it approved the pill Sovaldi in combination with older drugs to treat the main forms of hepatitis C that affect U.S. patients.
Current treatments for hepatitis C can take up to a year of therapy and involve weekly injections of a drug that causes flu-like side effects. That approach only cures about three out of four patients. Sovaldi is a daily pill that in clinical trials cured roughly 90 percent of patients in just 12 weeks, when combined with the older drug cocktail.http://www.pharmalive.com/us-approves-breakthrough-hepatitis-c-drug
- The end of October 2013 saw a nod from the FDA given to Gilead’s New Drug Application for Sofosbuvir, a much needed treatment for hepatitis C.
- As a nucleotide analogue, Sofosbuvir is designed as a once daily treatment.
- There are roughly 170 million cases of hepatitis C around the world.
- A report in the Journal of the American Medical Association on August 28, 2013 revealed that the Sofosbuvir and Ribavirin combination treatment effectively cured many patients with the Hepatitis C Virus.
- The Sofosbuvir and Ribavirin drug combination was void of interferon-based treatments, which many patients are resistant too.
- More than 3 million Americans have chronic Hepatitis C Virus, and 22 percent of these patients are African American.
Sofosbuvir (brand names Sovaldi and Virunon) is a drug used for hepatitis C virus (HCV) infection, with a high cure rate.[1][2] It inhibits the RNA polymerase that the hepatitis C virus uses to replicate its RNA. It was discovered at Pharmasset and developed by Gilead Sciences.[3]
Sofosbuvir is a component of the first all-oral, interferon-free regimen approved for treating chronic Hepatitis C.[4]
In 2013, the FDA approved sofosbuvir in combination with ribavirin (RBV) for oral dual therapy of HCV genotypes 2 and 3, and for triple therapy with injected pegylated interferon (pegIFN) and RBV for treatment-naive patients with HCV genotypes 1 and 4.[4] Sofosbuvir treatment regimens last 12 weeks for genotypes 1, 2 and 4, compared to 24 weeks for treatment of genotype 3. The label furhter states that sofosbuvir in combination with ribavirin may be considered for patients infected with genotype 1 who are interferon-ineligible.[5] Sofosbuvir will cost $84,000 for 12 weeks of treatment and $168,000 for the 24 weeks, which some patient advocates have criticized as unaffordable.
Interferon-free therapy for treatment of hepatitis C eliminates the substantial side-effects associated with use of interferon. Up to half of hepatitis C patients cannot tolerate the use of interferon.[6]
Sofosbuvir is a prodrug that is metabolized to the active antiviral agent 2′-deoxy-2′-α-fluoro-β-C-methyluridine-5′-triphosphate.[7] Sofosbuvir is anucleotide analog inhibitor of the hepatitis C virus (HCV) polymerase.[8] The HCV polymerase or NS5B protein is a RNA-dependent RNA polymerase critical for the viral cycle.
The New Drug Application for Sofosbuvir was submitted on April 8, 2013 and received the FDA’s Breakthrough Therapy Designation, which grants priority review status to drug candidates that may offer major treatment advantages over existing options.[9]
On 6th December 2013, the U.S. Food and Drug Administration approved sofosbuvir for the treatment of chronic hepatitis C.[10]
Sofosbuvir is being studied in combination with pegylated interferon and ribavirin, with ribavirin alone, and with other direct-acting antiviral agents.[11][12] It has shown clinical efficacy when used either with pegylated interferon/ribavirin or in interferon-free combinations. In particular, combinations of sofosbuvir with NS5A inhibitors, such as daclatasvir or GS-5885, have shown sustained virological response rates of up to 100% in people infected with HCV.[13]
Data from the ELECTRON trial showed that a dual interferon-free regimen of sofosbuvir plus ribavirin produced a 24-week post-treatment sustained virological response (SVR24) rate of 100% for previously untreated patients with HCV genotypes 2 or 3.[14][15]
Data presented at the 20th Conference on Retroviruses and Opportunistic Infections in March 2013 showed that a triple regimen of sofosbuvir, ledipasvir, and ribavirin produced a 12-week post-treatment sustained virological response (SVR12) rate of 100% for both treatment-naive patients and prior non-responders with HCV genotype 1.[16] Gilead has developed a sofosbuvir + ledipasvir coformulation that is being tested with and without ribavirin.
Sofosbuvir will cost $84,000 for 12 weeks of treatment used for genotype 1 and 2, and $168,000 for the 24 weeks used for genotype 3.[17] This represents a substantial pricing increase from previous treatments consisting of interferon and ribavirin, which cost between $15,000 and $20,000.[18] The price is also significantly higher than that of Johnson & Johnson‘s recently approved drug simeprevir (Olysio), which costs $50,000 and also treats chronic hepatitis C.[18] The high cost of the drug has resulted in a push back from insurance companies and the like, includingExpress Scripts, which has threatened to substitute lower priced competitors, even if those therapies come with a more unfriendly dosing schedule.[18] Other treatments that have recently entered the market have not matched the efficacy of sofosbuvir, however, allowing Gilead to set a higher price until additional competition enters the market.[18] Patient advocates such as Doctors Without Borders have complained about the price, which is particularly difficult for underdeveloped countries to afford.[19]
sofosbuvir
- News: United States to approve potent oral drugs for hepatitis C, Sara Reardon, Nature, 30 October 2013
- Sofia MJ, Bao D, Chang W, Du J, Nagarathnam D, Rachakonda S, Reddy PG, Ross BS, Wang P, Zhang HR, Bansal S, Espiritu C, Keilman M, Lam AM, Steuer HM, Niu C, Otto MJ, Furman PA (October 2010). “Discovery of a β-d-2′-deoxy-2′-α-fluoro-2′-β-C-methyluridine nucleotide prodrug (PSI-7977) for the treatment of hepatitis C virus”. J. Med. Chem. 53 (19): 7202–18.doi:10.1021/jm100863x. PMID 20845908.
- “PSI-7977”. Gilead Sciences.
- Tucker M (December 6, 2013). “FDA Approves ‘Game Changer’ Hepatitis C Drug Sofosbuvir”. Medscape.
- “U.S. Food and Drug Administration Approves Gilead’s Sovaldi™ (Sofosbuvir) for the Treatment of Chronic Hepatitis C – See more at: http://www.gilead.com/news/press-releases/2013/12/us-food-and-drug-administration-approves-gileads-sovaldi-sofosbuvir-for-the-treatment-of-chronic-hepatitis-c#sthash.T9uTbSWK.dpuf”. Gilead. December 6, 2013.
- “Sofosbuvir is safer than interferon for hepatitis C patients, say scientists”. News Medical. April 25, 2013.
- Murakami E, Tolstykh T, Bao H, Niu C, Steuer HM, Bao D, Chang W, Espiritu C, Bansal S, Lam AM, Otto MJ, Sofia MJ, Furman PA (November 2010). “Mechanism of activation of PSI-7851 and its diastereoisomer PSI-7977”. J. Biol. Chem. 285 (45): 34337–47.doi:10.1074/jbc.M110.161802. PMC 2966047. PMID 20801890.
- Alejandro Soza (November 11, 2012). “Sofosbuvir”. Hepaton.
- “FDA Advisory Committee Supports Approval of Gilead’s Sofosbuvir for Chronic Hepatitis C Infection”. Drugs.com. October 25, 2013.
- “FDA approves Sovaldi for chronic hepatitis C”. FDA New Release. U.S. Food and Drug Administration. 2013-12-06.
- Murphy T (November 21, 2011). “Gilead Sciences to buy Pharmasset for $11 billion”.Bloomberg Businessweek.
- Asselah T (January 2014). “Sofosbuvir for the treatment of hepatitis C virus”. Expert Opin Pharmacother 15 (1): 121–30. doi:10.1517/14656566.2014.857656. PMID 24289735.
- “AASLD 2012: Sofosbuvir and daclatasvir dual regimen cures most people with HCV genotypes 1, 2, or 3”. News. European Liver Patients Association. 2012-11-21.
- AASLD: PSI-7977 plus Ribavirin Can Cure Hepatitis C in 12 Weeks without Interferon. Highleyman, L. HIVandHepatitis.com. 8 November 2011.
- Gane EJ, Stedman CA, Hyland RH, Ding X, Svarovskaia E, Symonds WT, Hindes RG, Berrey MM (January 2013). “Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C”.N. Engl. J. Med. 368 (1): 34–44. doi:10.1056/NEJMoa1208953. PMID 23281974.
- CROI 2013: Sofosbuvir + Ledipasvir + Ribavirin Combo for HCV Produces 100% Sustained Response. Highleyman, L. HIVandHepatitis.com. 4 March 2013.
- Campbell T (December 11, 2013). “Gilead’s Sofosbuvir Gets New Name, Price, Headaches”. The Motley Fool.
- Cohen, J. (2013). “Advocates Protest the Cost of a Hepatitis C Cure”. Science 342 (6164): 1302–1303. doi:10.1126/science.342.6164.1302. PMID 24337268. edit
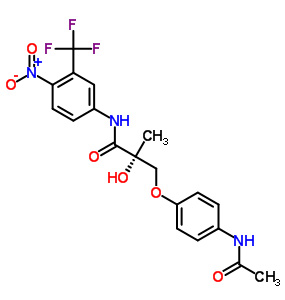
The chemical structure

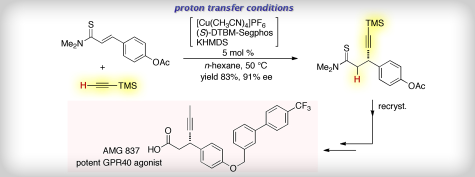
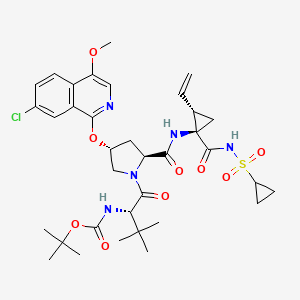
GS-7977, (S)-isopropyl 2-(((S)-(((2R,3R,4R,5R)-5-(2,4-dioxo-3,4- dihydropyrimidin^l(2H)-yl)-4-fluoro-3-hydroxy-4-methyltetrahydrofuran-2- yl)methoxy)(phenoxy)phosphoryl)amino)propanoate, available from Gilead Sciences, Inc., is described and claimed in U.S. Patent No. 7,964,580. (See also US 2010/0016251, US 2010/0298257, US 201 1/0251 152 and US 2012/0107278.) GS-7977 has the structure:
GS-7977 can be crystalline or amorphous. Examples of preparing crystalline and amorphous forms of GS-7977 are disclosed in US 2010/0298257 (US 12/783,680) and US 201 1/0251 152 (US 13/076,552),

Commerically available isopropylidine protected D-glyceraldehyde was reacted with (carbethoxyethylidene)triphenylmethylphosphorane gave the chiral pentenoate ester YP-1. Permanganate dihydroxylation of YP-1 in acetone gave the D-isomer diol YP-2. The cyclic sulfate YP-3 was obtained by first making the cyclic sulfite with thionyl chloride and then oxidizing to cyclic sulfate with sodium hypochlorite. Fluorination of YP-3 with triethylamine-trihydrofluoride(TEA-3HF) in the presence of triethylamine, followed by the hydrolysis of sulfate ester in the presence of concentrated HCl provided diol YP-4 which was benzoylated to give ribonolactone YP-5. Reduction of YP-5 with Red-Al followed by chlorination with sulfuryl chloride in the presence of catalytic amount of tetrabutylammonium bromide yielded YP-6. The conversion of YP-6 to benzoyl protected 2′-deoxyl-2′-alpha-F-2′-Beta-C-methylcytidine (YP-7) was achieved by using O-trimethyl silyl-N4-benzoylcytosine and stannic chloride. Preparation of the uridine nucleoside YP-8 was accomplished by first heating benzoyl cytidine YP-7 in acetic acid then treating with methoanolic ammonia to provide YP-8 in 78% yield.
The phosphoramidating reagent YP-9 was obtained by first reacting phenyldichlorophosphate with L-Alanine isopropyl ester hydrochloride and then with pentafluorophenol. Isolation of single Sp diastereomer YP-9 was achieved via crystallization-induced dynamic resolution in the presence of 20% MTBE/hexane at room temperature.
The uridine nucleoside YP-8 was treated with tert-butylmagnesium chloride in dry THF, followed by pentafluorophenyl Sp diastereomer YP-9 to furnish the Isopropyl (2S)-2-[[[(2R,3R,4R,5R)-5-(2,4-dioxopyrimidin-1-yl)-4-fluoro-3-hydroxy-4-methyl-tetrahydrofuran-2-yl]methoxy-phenoxy-phosphoryl]amino]propanoate (Sovaldi, sofosbuvir, GS-7977, PSI-7977)。
…………
US 7429572
US 8415322
US 7964580
US 8334270B
WO 2006012440
WO 2011123668
US8334270
/US20080139802
……………………………………………
In US 20050009737 published Jan. 13, 2005, J. Clark discloses fluoro-nucleoside derivatives that inhibit Hepatitis C Virus (HCV) NS5B polymerase. In particular, 4-amino-1-((2R,3R,4R,5R)-3-fluoro-4-hydroxy-5-hydroxymethyl-3-methyl-tetrahydro-faran-2-yl)-1H-pyrimidin-2-one (18) was a particularly potent inhibitor of HCV polymerase as well as the polymerase of other Flaviviridae.

In WO2006/012440 published Feb. 2, 2006, P. Wang et al disclose processes for the preparation of 18. Introduction of the cytosine is carried out utilizing the Vorbruggen protocol. In US 20060122146 published Jun. 8, 2006, B.-K. Chun et al. disclose and improved procedures for the preparation of the 2-methyl-2-fluoro-lactone 10. In the latter disclosure the nucleobase is glycosylated by reacting with ribofuranosyl acetate which is prepared by reduction of 10 with LiAlH(O-tert-Bu)3 followed by acetylaton of the intermediate lactol which was treated with an O-trimethylsilyl N4-benzoylcytosine in the presence of SnCl4 to afford the O,O,N-tribenzoylated nucleoside.
……………………………………………………………….
http://www.google.nl/patents/US20080139802
The present process as described in SCHEME A and the following examples contain numerous improvements which have resulted in higher yields of the desired nucleoside. The asymmetric hydroxylation of 22 was discovered to be best carried out with sodium permanganate in the presence of ethylene glycol, sodium bicarbonate in acetone which afforded the diol in 60-64% on pilot plant scale. The sodium permanganate procedure avoids introduction of osmium into the process stream. Further more the stereospecific hydroxylation can be accomplished without using an expensive chiral ligand. The requisite olefin is prepared from (1S,2S)-1,2-bis-((R)-2,2-dimethyl-[1,3]dioxolan-4-yl)-ethane-1,2-diol (20) (C. R. Schmid and J. D. Bryant, Org. Syn. 1995 72:6-13) by oxidative cleavage of the diol and treating the resulting aldehyde with 2-(triphenyl-λ5-phosphanylidene)-propionic acid ethyl ester to afford 22.

(i) NaIO4, NaHCO3, DCM; (ii) MeC(═PPh3)CO2Et; (iii) acetone-NaMnO4 (aq), ethylene glycol, NaHCO3, −10 to 0° C.; aq. NaHSO3 (quench); (iv) i-PrOAc, MeCN, TEA, SOCl2; (v) i-PrOAc, MeCN, NaOCl; (vi) TEA-3HF, TEA; (vii) HCl (aq)-BaCl2-aq; (viii) (PhCO)2O, DMAP, MeCN, (ix) RED-AL/TFE (1:1), DCM; (x) SO2Cl2-TBAB, DCM; (xi) 32, SnCl4-PhCl; (xii) MeOH-MeONa
EXAMPLE 3 (2S,3R)-3-[(4R)-2,2-dimethyl-[1,3]dioxolan-4-yl]-2,3-dihydroxy-2-methyl-propionic acid ethyl ester (24)

A suspension of 22 (10 kg, CAS Reg. No. 81997-76-4), ethylene glycol (11.6 kg), solid NaHCO3 (11.8 kg) and acetone (150 L) is cooled to ca.-15° C. A solution of 36% aqueous NaMnO4 (19.5 kg) is charged slowly (over 4 h) to the suspension maintaining reaction temperature at or below −10° C. After stirring for 0.5 h at −10° C., an aliquot of the reaction mixture (ca. 5 mL) is quenched with 25% aqueous sodium bisulfite (ca. 15 mL). A portion of resulting slurry is filtered and submitted for GC analysis to check the progress of the reaction. When the reaction is complete, the reaction mixture is quenched by slow addition (over 40 min) of cooled (ca. 0° C.) 25% aqueous NaHSO3 (60 L). The temperature of the reaction mixture is allowed to reach 4° C. during the quench. CELITE® (ca. 2.5 kg) is then slurried in acetone (8 kg) and added to the dark brown reaction mixture. The resulting slurry is aged at RT to obtain light tan slurry. The slurry is filtered, and the filter cake is washed with acetone (3×39 kg). The combined filtrate is concentrated by vacuum distillation (vacuum approximately 24 inches of Hg; max pot temperature is 32° C.) to remove the acetone. The aqueous concentrate is extracted with EtOAc (3×27 kg), and the combined organic extracts were washed with water (25 L). The organic phase is then concentrated by atmospheric distillation and EtOAc is replaced with toluene. The volume of the batch is adjusted to ca. 20 L. Heptane (62 kg) is added and the batch cooled to ca. 27° C. to initiate crystallization. The batch is then cooled to −10° C. After aging overnight at −10° C., the product is filtered, washed with 10% toluene in heptane and dried at 50° C. under vacuum to afford 6.91 kg (59.5%) of 24 (CARN 81997-76-4) as a white crystalline solid.
EXAMPLE 4 (3R,4R,5R)-3-Fluoro-4-hydroxy-5-hydroxymethyl-3-methyl-dihydro-furan-2-one (10)

steps 1 & 2—A dry, clean vessel was charged with 24 (6.0 kg), isopropyl acetate (28.0 kg), MeCN (3.8 kg) and TEA (5.4 kg). The mixture was cooled to 5-10° C., and thionyl chloride (3.2 kg) was added slowly while cooling the solution to maintain the temperature below 20° C. The mixture was stirred until no starting material was left (GC analysis). The reaction was typically complete within 30 min after addition is complete. To the mixture was added water (9 kg) and after stirring, the mixture was allowed to settle. The aqueous phase was discarded and the organic phase was washed with a mixture of water (8 kg) and saturated NaHCO3 (4 kg) solution. To the remaining organic phase containing 36 was added MeCN (2.5 kg) and solid NaHCO3 (3.1 kg). The resulting slurry was cooled to ca. 10° C. Bleach (NaOCl solution, 6.89 wt % aqueous solution, 52.4 kg, 2 eq.) was added slowly while cooling to maintain temperature below 25° C. The mixture was aged with stirring over 90-120 min at 20-25° C., until the reaction was complete (GC analysis). After completion of the reaction, the mixture was cooled to ca. 10° C. and then quenched with aqueous Na2SO3 solution (15.1% w/w, 21 kg) while cooling to maintain temperature below 20° C. The quenched reaction mixture was filtered through a cartridge filter to remove inorganic solids. The filtrate was allowed to settle, and phases are separated and the aqueous phase is discarded. The organic layer was washed first with a mixture of water (11 kg) and saturated NaHCO3 solution (4.7 kg), then with of saturated NaHCO3 solution (5.1 kg). DIPEA (220 mL) was added to the organic phase and the resulting solution was filtered through CELITE® (bag filter) into a clean drum. The reactor was rinsed with isopropyl acetate (7 kg) and the rinse is transferred to the drum. The organic phase was then concentrated under vacuum (25-28 inches of Hg) while maintaining reactor jacket temperature at 45-50° C. to afford 26 as an oil (˜10 L). Additional DIPEA (280 mL) was added and the vacuum distillation was continued (jacket temperature 50-55° C.) until no more distillate was collected. (batch volume ca. 7 L).
step 3—To the concentrated oil from step 2 containing 26 was added TEA (2.34 kg) and TEA-trihydrofluoride (1.63 kg). The mixture was heated to 85° C. for 2 h. The batch was sampled to monitor the progress of the reaction by GC. After the reaction was complete conc. HCl (2.35 kg) was added to the mixture and the resulting mixture heated to ca. 90° C. (small amount of distillate collected). The reaction mixture was stirred at ca. 90° C. for 30 min and then saturated aqueous BaCl2solution (18.8 kg) was added. The resulting suspension was stirred at about 90° C. for 4 h. The resulting mixture was then azeotropically dried under a vacuum (9-10 inches of Hg) by adding slowly n-propanol (119 kg) while distilling off the azeotropic mixture (internal batch temperature ca. 85-90° C.). To the residual suspension was added toluene (33 kg) and vacuum distillation was continued to distill off residual n-propanol (and traces of water) to a minimum volume to afford 28.
step 4—To the residue from step 3 containing 28 was added MeCN (35 kg) and ca. 15 L was distilled out under atmospheric pressure. The reaction mixture was cooled to ca. 10° C. and then benzoyl chloride (8.27 kg) and DMAP (0.14 kg) are added. TEA (5.84 kg) was added slowly to the reaction mixture while cooling to maintain temperature below 40° C. The batch was aged at ca. 20° C. and the progress of the benzoylation is monitored by HPLC. After completion of the reaction, EtOAc (30 kg) was added to the mixture and the resulting suspension is stirred for about 30 min. The reaction mixture was filtered through a CELITE® pad (using a nutsche filter) to remove inorganic salts. The solid cake was washed with EtOAc (38 kg). The combined filtrate and washes were washed successively with water (38 kg), saturated NaHCO3 solution (40 kg) and saturated brine (44 kg). The organic phase was polish-filtered (through a cartridge filter) and concentrated under modest vacuum to minimum volume. IPA (77 kg) was added to the concentrate and ca. 25 L of distillate was collected under modest vacuum allowing the internal batch temperature to reach ca. 75° C. at the end of the distillation. The remaining solution was then cooled to ca. 5° C. over 5 h and optionally aged overnight. The precipitate was filtered and washed with of cold (ca. 5° C.) IPA (24 kg). The product was dried under vacuum at 60-70° C. to afford 6.63 kg (70.7% theory of 10 which was 98.2% pure by HPLC.
EXAMPLE 1 Benzoic acid 3-benzoyloxy-5-(4-benzoylamino-2-oxo-2H-pyrimidin-1-yl)-4-fluoro-4-methyl-tetrahydro-furan-2-ylmethyl ester (14)

Trifluoroethanol (4.08 kg) is added slowly to a cold solution (−15° C.) of RED-AL® solution (12.53 kg) and toluene (21.3 kg) while maintaining the reaction temperature at or below −10° C. After warming up to RT (ca. 20° C.), the modified RED-AL reagent mixture (30.1 kg out of the 37.6 kg prepared) is added slowly to a pre-cooled solution (−15° C.) of fluorolactone dibenzoate 10 (10 kg) in DCM (94.7 kg) while maintaining reaction temperature at or below −10° C. After reduction of the lactone (monitored by in-process HPLC), a catalytic amount of tetrabutylammonium bromide (90 g) is added to the reaction mixture. Sulfiiryl chloride (11.86 kg) is then added while maintaining reaction temperature at or below 0° C. The reaction mixture is then heated to 40° C. until formation of the chloride is complete (ca. 4 h) or warmed to RT (20-25° C.) and stirred over night (ca. 16 h). The reaction mixture is cooled to about 0° C., and water (100 L) is added cautiously while maintaining reaction temperature at or below 15° C. The reaction mixture is then stirred at RT for ca. 1 h to ensure hydrolytic decomposition of excess sulfuryl chloride and the phases are separated. The organic layer is washed with a dilute solution of citric acid (prepared by dissolving 15.5 kg of citric acid in 85 L of water) and then with dilute KOH solution (prepared by dissolving 15 kg of 50% KOH in 100 L of water). The organic phase is then concentrated and solvents are replaced with chlorobenzene (2×150 kg) via atmospheric replacement distillation. The resulting solution containing 30 is dried azeotropically.
A suspension of N-benzoyl cytosine (8.85 kg), ammonium sulfate (0.07 kg) and hexamethyldisilazane (6.6 kg) in chlorobenzene (52.4 kg) is heated to reflux (ca. 135° C.) and stirred (ca. 1 h) until the mixture becomes a clear solution. The reaction mixture is then concentrated in vacuo to obtain 32 as a syrupy liquid. The anhydrous solution of 30 in chlorobenzene (as prepared) and stannic chloride (28.2 kg) is added to this concentrate. The reaction mixture is maintained at about 70° C. until the desired coupling reaction is complete (ca. 10 h) as determined by in-process HPLC. Upon completion, the reaction mixture is cooled to RT and diluted with DCM (121 kg). This solution is added to a suspension of solid NaHCO3 (47 kg) and CELITE® (9.4 kg) in DCM (100.6 kg). The resulting slurry is cooled to 10-15° C., and water (8.4 kg) is added slowly to quench the reaction mixture. The resulting suspension is very slowly (caution: gas evolution) heated to reflux (ca. 45° C.) and maintained for about 30 min. The slurry is then cooled to ca. 15° C. and filtered. The filter cake is repeatedly reslurried in DCM (4×100 L) and filtered. The combined filtrate is concentrated under atmospheric pressure (the distillate collected in the process is used for reslurrying the filter cake) until the batch temperature rises to about 90° C. and then allowed to cool slowly to about −5° C. The resulting slurry is aged for at least 2 h at −5° C. The precipitated product is filtered and washed with IPA (30 kg+20 kg), and oven-dried in vacuo at about 70° C. to afford 8.8 kg (57.3%) of 1-(2-deoxy-2-fluoro-2-methyl-3-5-O-dibenzoyl-β-D-ribofuranosyl)-N-4-benzoylcytosine (14, CAS Reg No. 817204-32-3) which was 99.3% pure.
EXAMPLE 2 4-Amino-1-(3-fluoro-4-hydroxy-5-hydroxymethyl-3-methyl-tetrahydro-furan-2-yl)-1H-pyrimidin-2-one (18)
A slurry of 14 (14.7 kg) in MeOH (92.6 kg) is treated with catalytic amounts of methanolic sodium methoxide (0.275 kg). The reaction mixture is heated to ca. 50° C. and aged (ca. 1 h) until the hydrolysis is complete. The reaction mixture is quenched by addition of isobutyric acid (0.115 kg). The resulting solution is concentrated under moderate vacuum and then residual solvents are replaced with IPA (80 kg). The batch is distilled to a volume of ca. 50 L. The resulting slurry is heated to ca. 80° C. and then cooled slowly to ca. 5° C. and aged (ca. 2 h). The precipitated product is isolated by filtration, washed with IPA (16.8 kg) and dried in an oven at 70° C. in vacuo to afford 6.26 kg (88.9%) of 18 which assayed at 99.43% pure.
………………………………………………………………………
https://www.google.com/patents/US8334270
EXAMPLE 4 Preparation of 2′-deoxy-2′-fluoro-2′-C-methyluridine

2′-Deoxy-2′-fluoro-2′-C-methylcytidine (1.0 g, 1 eq) (Clark, J., et al., J. Med. Chem., 2005, 48, 5504-5508) was dissolved in 10 ml of anhydrous pyridine and concentrated to dryness in vacuo. The resulting syrup was dissolved in 20 ml of anhydrous pyridine under nitrogen and cooled to 0° C. with stirring. The brown solution was treated with benzoyl chloride (1.63 g, 3 eq) dropwise over 10 min. The ice bath was removed and stirring continued for 1.5 h whereby thin-layer chromatography (TLC) showed no remaining starting material. The mixture was quenched by addition of water (0.5 ml) and concentrated to dryness. The residue was dissolved in 50 mL of dichloromethane (DCM) and washed with saturated NaHCO3 aqueous solution and H2O. The organic phase was dried over NaSO4 and filtered, concentrated to dryness to give N4,3′,5′-tribenzoyl-2′-Deoxy-2′-fluoro-2′-C-methylcytidine (2.0 g, Yield: 91%).
N4,3′,5′-tribenzoyl-2′-Deoxy-2′-fluoro-2′-C-methylcytidine (2.0 g, 1 eq) was refluxed in 80% aqueous AcOH overnight. After cooling and standing at room temperature (15° C.), most of the product precipitated and then was filtered through a sintered funnel. White precipitate was washed with water and co-evaporated with toluene to give a white solid. The filtrate was concentrated and co-evaporated with toluene to give additional product which was washed with water to give a white solid. Combining the two batches of white solid gave 1.50 g of 3′,5′-dibenzoyl-2′-Deoxy-2′-fluoro-2′-C-methyluridine (Yield: 91%).
To a solution of 3′,5′-dibenzoyl-2′-Deoxy-2′-fluoro-2′-C-methyluridine (1.5 g, 1 eq) in MeOH (10 mL) was added a solution of saturated ammonia in MeOH (20 mL). The reaction mixture was stirred at 0° C. for 30 min, and then warmed to room temperature slowly. After the reaction mixture was stirred for another 18 hours, the reaction mixture was evaporated under reduced pressure to give the residue, which was purified by column chromatography to afford pure compound 2′-deoxy-2′-fluoro-2′-C-methyluridine (500 mg, Yield: 60%).
Example numbers 13-54 and 56-66 are prepared using similar procedures described for examples 5-8. The example number, compound identification, and NMR/MS details are shown below:
| entry 251H NMR (DMSO-d6) δ 1.13-1.28 (m, 12H), 3.74-3.81 (m, 2H), 3.95-4.08 (m, 1H), 4.20-4.45 (m, 2H), 4.83-4.87 (m, 1H), 5.52-5.58 (m, 1H),5.84-6.15 (m, 3H), 7.17-7.23 (m, 3H), 7.35-7.39 (m, 2H), 7.54-7.57(m, 1H), 11.50 (s. 1H); MS, m/e 530.2 (M + 1)+ |
|
|
|
|
|
|
|
Discovery of a β-d-2′-deoxy-2′-α-fluoro-2′-β-C-methyluridine nucleotide prodrug (PSI-7977) for the treatment of hepatitis C virus.
Sofia MJ, Bao D, Chang W, Du J, Nagarathnam D, Rachakonda S, Reddy PG, Ross BS, Wang P, Zhang HR, Bansal S, Espiritu C, Keilman M, Lam AM, Steuer HM, Niu C, Otto MJ, Furman PA.
J Med Chem. 2010 Oct 14;53(19):7202-18. doi: 10.1021/jm100863x.
Mechanism of activation of PSI-7851 and its diastereoisomer PSI-7977.
Murakami E, Tolstykh T, Bao H, Niu C, Steuer HM, Bao D, Chang W, Espiritu C, Bansal S, Lam AM, Otto MJ, Sofia MJ, Furman PA.
J Biol Chem. 2010 Nov 5;285(45):34337-47. doi: 10.1074/jbc.M110.161802. Epub 2010 Aug 26.
Michael J. Sofia,Donghui Bao, Wonsuk Chang, Jinfa Du, Dhanapalan Nagarathnam, Suguna Rachakonda, P. Ganapati Reddy, Bruce S. Ross, Peiyuan Wang, Hai-Ren Zhang, Shalini Bansal, Christine Espiritu, Meg Keilman, Angela M. Lam, Holly M. Micolochick Steuer, Congrong Niu, Michael J. Otto, and Phillip A. Furman; Discovery of a β-D-2’-Deoxy-2’-a-fluoro-2’-β-C-methyluridine Nucleotide Prodrug (PSI-7977) for the Treatment of Hepatitis C Virus; J. Med. Chem. 2010, 53, 7202–7218; Pharmasset, Inc.
Bruce S. Ross, P. Ganapati Reddy , Hai-Ren Zhang , Suguna Rachakonda , and Michael J. Sofia; Synthesis of Diastereomerically Pure Nucleotide Phosphoramidates; J. Org. Chem., 2011, 76 (20), pp 8311–8319; Pharmasset, Inc.
Peiyuan Wang, Byoung-Kwon Chun, Suguna Rachakonda, Jinfa Du, Noshena Khan, Junxing Shi, Wojciech Stec, Darryl Cleary, Bruce S. Ross and Michael J. Sofia; An Efficient and Diastereoselective Synthesis of PSI-6130: A Clinically Efficacious Inhibitor of HCV NS5B Polymerase; J. Org. Chem., 2009, 74 (17), pp 6819–6824;Pharmasset, Inc.
Jeremy L. Clark, Laurent Hollecker, J. Christian Mason, Lieven J. Stuyver, Phillip M. Tharnish, Stefania Lostia, Tamara R. McBrayer, Raymond F. Schinazi, Kyoichi A. Watanabe, Michael J. Otto, Phillip A. Furman, Wojciech J. Stec, Steven E. Patterson, and Krzysztof W. Pankiewicz; Design, Synthesis, and Antiviral Activity of 2‘-Deoxy-2‘-fluoro-2‘-C-methylcytidine, a Potent Inhibitor of Hepatitis C Virus Replication; J. Med. Chem., 2005, 48 (17), pp 5504–5508; Pharmasset, Inc
- Harrison C. Patent battle lines drawn as sofosbuvir gains approval. , Nat Rev Drug Discov , Volume 13 , Issue 1 , 2013 Dec 31
- Traynor K. Sofosbuvir approved for chronic hepatitis C infection. , Am J Health Syst Pharm , Volume 71 , Issue 2 , 2014 Jan 15
- Benhamou Y. HCV F1/F2 patients: treat now or continue to wait. , Liver Int , Volume 34 Suppl 1 , 2014 Feb
- Asselah T. HCV direct-acting antiviral agents: the best interferon-free combinations. , Liver Int , Volume 34 Suppl 1 , 2014 Feb
- Marcellin P. Second-wave IFN-based triple therapy for HCV genotype 1 infection: simeprevir, faldaprevir and sofosbuvir. , Liver Int , Volume 34 Suppl 1 , 2014 Feb
- Corouge M. Treatment of hepatitis C virus genotype 3-infection. , Liver Int , Volume 34 Suppl 1 , 2014 Feb
- Osinusi A. IFNL4-ΔG Genotype is Associated with Slower Viral Clearance in Hepatitis C, Genotype-1 Patients Treated with Sofosbuvir and Ribavirin. , J Infect Dis , 2013 Dec 23
- Alavian SM. Sofosbuvir has come out of the magic box. , Hepat Mon , Volume 13 , Issue 12 , 2013 Dec 16
- Ferguson MC. Sofosbuvir with ribavirin is safe and effective in hepatitis C genotype 1 with unfavourable pretreatment characteristics. , Evid Based Med , 2013 Dec 12
- Hunt S. Minimal Impact of Sofosbuvir and Ribavirin on Health Related Quality of Life in Chronic Hepatitis C (CH-C). , J Hepatol , 2013 Dec 10
SOVALDI is the brand name for sofosbuvir, a nucleotide analog inhibitor of HCV NS5B polymerase.
The IUPAC name for sofosbuvir is (S)-Isopropyl 2-((S)-(((2R,3R,4R,5R)-5-(2,4-dioxo-3,4-dihydropyrimidin-1(2H)-yl)-4-fluoro-3-hydroxy-4-methyltetrahydrofuran-2-yl)methoxy)-(phenoxy)phosphorylamino)propanoate. It has a molecular formula of C22H29FN3O9P and a molecular weight of 529.45. It has the following structural formula:
Sofosbuvir is a white to off-white crystalline solid with a solubility of ≥ 2 mg/mL across the pH range of 2-7.7 at 37 oC and is slightly soluble in water.
SOVALDI tablets are for oral administration. Each tablet contains 400 mg of sofosbuvir. The tablets include the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, mannitol, and microcrystalline cellulose. The tablets are film-coated with a coating material containing the following inactive ingredients: polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide, and yellow iron oxide.
DO NOT FORGET TO CLICK
SEE………………….http://orgspectroscopyint.blogspot.in/2015/02/sofosbuvir-visited.html
J. Med. Chem. 2005, 48, 5504.
WO2008045419A1
CN201180017181

(WO2015139602) 2′-SUBSTITUTED-2,2′-DEHYDRATED URIDINE OR 2′-SUBSTITUTED-2,2′-DEHYDRATED CYTIDINE COMPOUND AND PREPARATION METHOD AND USE THEREOF
ZHANG, Rongxia
A further object of the present invention to provide a method for preparing a compound of formula I.
The present invention provides a process for preparing a compound I 2′-deoxy-2′-fluoro-2′-substituted uridine or 2′-deoxy-2′-fluoro-cytidine using the following formula or 2′-deoxy-2′-substituted 2′-2′-substituted nitrile or uridine 2′-deoxy-2′-substituted-2′-carbonitrile The method of cytidine compound,
2′-deoxy-2′-fluoro-2′-methyl-uridine (IIIa) is the preparation of anti-hepatitis C drugs Sofosbuvir key intermediate.
Sofosbuvir developed by Gilead Science Company, FDA on December 6, 2013 Sofosbuvir formally approved for the treatment of chronic hepatitis C virus (HCV) infection. Sofosbuvir is first used to treat certain types of HCV infection without the use of interferon effective and safe drugs. Clinical trials have shown, sofosbuvir can achieve very high proportion of sustained virologic response (clinical cure). More revolutionary breakthrough that, sofosbuvir without joint peginterferon α situation is still very significant effect, such as sofosbuvir ribavirin genotype 2 and genotype 3 patients with previously untreated chronic hepatitis C continued virological response rate of 100%. Sofosbuvir is a prodrug is metabolized in vivo to 2′-deoxy-2′-fluoro-2′-methyl-uridine-5′-monophosphate.
Currently reported 2′-deoxy-2′-fluoro-2′-methyl uridine synthetic methods are as follows:
In the literature (Journal of Medicinal Chemistry, 2005,48,5504) in order cytidine as a raw material, first selectively protected 3 ‘, 5′-hydroxyl group, and then oxidizing the 2′-hydroxyl to a carbonyl group, and the reaction of methyllithium get the 2’-hydroxyl compound, and then removing the protective group, use benzoyl protected 3 ‘, 5’-hydroxyl group, and then reacted with DAST fluorinated compound, followed by hydrolysis and aminolysis reaction products, such as the following Reaction Scheme. The method of route length, the need to use expensive silicon ether protecting group molecule relatively poor economy; conducting methylation time will generate a non-methyl enantiomer beta bits.
In Patent (WO2005003147, WO2006031725A2, US20040158059) using 2′-fluoro-2′-methyl – ribose derivative with N- benzoyl cytosine for docking the reaction, then after the hydrolysis, aminolysis reaction to obtain the final product, As shown in the following reaction scheme. Raw material of the process is not readily available, synthetic steps cumbersome, expensive; the reaction product obtained contained docking base for the alpha position isomers, need purification removed to form waste.
The present inventors have designed and synthesized a compound of formula I as shown, the compound may be a fluorinated or nitrile reaction of 2′-deoxy-2′-fluoro-2′-get-substituted uridine or 2 under appropriate conditions’ – 2′-deoxy-2′-fluoro-2′-deoxy-2′-substituted cytidine or nitrile uridine or 2′-substituted-2′-deoxy-2′-substituted-2′-cytidine nitrile compound; or a compound of formula I or a nitrile group by fluoro reaction, followed by deprotection reaction to give 2′-deoxy-2′-fluoro-2′-substituted uridine or 2′-deoxy-2′-fluoro–2 ‘- cytidine or 2′-substituted-2′-deoxy-2′-nitrile-substituted uridine or 2′-deoxy-2′-substituted-2′-cytidine compound nitrile group; or a compound of formula I through the opening cyclization reaction, and then through the group of fluoro or nitrile, and finally deprotection reaction to give 2′-deoxy-2′-fluoro-2′-substituted uridine or 2′-deoxy-2′-fluoro-2’-substituted Cellular glycoside or 2 ‘substituted-2′-deoxy-2′-carbonitrile 2′-deoxy-uridine or 2′-substituted-2’-cytidine compound nitrile group; or a compound of formula I through a ring-opening reaction, and then 2 ‘- hydroxyl forming a leaving group, and then after a nitrile group or a fluorinated reaction, the final deprotection reaction of 2′-deoxy-2′-fluoro-2′-substituted uridine or 2′-deoxy-2′- cytidine or 2′-fluoro-2′-substituted-2′-deoxy-2′-nitrile-substituted uridine or 2′-deoxy-2′-substituted-2’-cytidine nitrile compound.
It is therefore an object of the present invention is to provide a compound of the general formula I prepared 2′-deoxy-2′-fluoro-2′-substituted uridine or 2′-deoxy-2′-fluoro-2′-substituted cytidine or 2′-substituted-2′-deoxy-2′-carbonitrile uridine or 2′-deoxy-2′-substituted-2′-carbonitrile The method of cytidine compound.
The 2′-C- methyl uridine (18.4g, 0.07mol), N, N’- carbonyldiimidazole (216.2g, 0.10mol), sodium bicarbonate (8.4g, 0.10mol) was suspended N, N- two dimethylformamide (50ml), the temperature was raised to 130 ℃, reaction for 4 hours, cooled and filtered to remove inorganic salts, the filtrate was added ethyl acetate (200ml), analyze the material at room temperature, suction filtered, washed with ethyl acetate cooled to, drying to give a yellow solid (19.9g, yield: 83%).
Ia: 1 H NMR (300 MHz, CD 3 OD): [delta] 7.80 (d, 1H, J = 7.5 Hz), 6.05 (d, 1H, J = 7.5 Hz), 5.91 (s, 1H), 4.34 (d, 1H, J = 4.8Hz), 4.07 (m, 1H), 3.56 (m, 2H), 1.63 (s, 3H); ESI-MS m / z (M + 1) 241.
The compound of Example 1 Ia (0.24g, 1mmol)) was dissolved in 70% HF in pyridine was heated to 140 ~ 150 ℃, stirred for 3 hours, cooled and the solvent was removed under reduced pressure, the residue was added acetone, beating, and filtered to give solid (0.18g, yield: 70%).
IIIa: 1 H NMR (300 MHz, DMSO-d 6 ): [delta] 11.48 (s, 1H), 7.82 (d, 1H, J = 6.0 Hz), 6.00 (d, 1H, J = 15.6 Hz), 5.67 (m , 2H), 5.30 (s, 1H), 3.85 (m, 3H), 3.62 (s, 1H), 1.25 (d, 3H, J = 16.8Hz), ESI-MS m / z (M-1) 259.
Compound Ib (0.45g, 1mmol) was dissolved in a mixture of dichloromethane and pyridine, was added DAST (0.32g), stirred for 24 hours, added dichloromethane (20ml) was diluted with water (30ml × 2), dried over anhydrous dried over sodium sulfate, filtered and the solvent removed under reduced pressure to give the residue was subjected to column chromatography to give the product (0.36g, yield: 78%).
IIa: 1 H NMR (400 MHz, CDCl 3 and DMSO-d 6 ): [delta] 7.99 (d, J = 7.6 Hz, 2H), 7.90 (d, J = 7.6 Hz, 2H), 7.34 ~ 7.61 (m, 7H ), 6.10 (brs, 1H), 5.64 (brs, 1H), 5.42 (d, J = 8.0Hz, 1H), 4.53-4.68 (m, 3H), 1.40 (d, J = 22.8Hz, 3H); ESI -MS m / z (M + 1) 469.
The compound of Example 3 IIa (0.47g, 1mmol) dissolved in 10% methanol solution of ammonia and stirred overnight, the solvent was removed under reduced pressure, and the residue was slurried in ethyl acetate, filtered to give a white solid (0.2g, yield : 77%).
IIIa: 1 H NMR (300 MHz, DMSO-d 6 ): [delta] 11.48 (s, 1H), 7.82 (d, 1H, J = 6.0 Hz), 6.00 (d, 1H, J = 15.6 Hz), 5.67 (m , 2H), 5.30 (s, 1H), 3.85 (m, 3H), 3.62 (s, 1H), 1.25 (d, 3H, J = 16.8Hz), ESI-MS m / z (M-1) 259.
Compound IVa (0.57g, 1mmol) was dissolved in dichloroethane (20ml) was added trifluoromethanesulfonic acid trimethylsilyl ester (1ml), was heated for 12 hours, cooled, and the reaction solution was concentrated dryness, added two dichloromethane (100ml) was dissolved, washed successively with water (50ml) and saturated brine (50ml), dried over anhydrous sodium sulfate, filtered, and the filtrate was concentrated to dryness to give an oil which was purified by column chromatography to give a white solid (0.3g, yield : 67%).
Ib: 1 H NMR (300 MHz, CDCl 3 ): δ7.96-8.10 (m, 6H), 7.41-7.65 (m, 9H), 7.32 (d, 1H, J = 5.4 Hz), 6.09 (d, 1H, J = 5.4Hz), 5.79 (m, 2H), 4.67 (m, 1H), 4.48 (m, 2H), 1.81 (s, 3H); ESI-MS m / z (M-1) 447.
N The compound of Example 1 Ia (1.3g, 5.4mmol) dissolved in dry, N- dimethylformamide (10ml) was added p-toluenesulfonic acid monohydrate (1.12g, 5.9mmol) and 3,4- dihydropyran (1.28ml, 14.04mmol), The reaction was stirred for 5 hours at room temperature, water was added and the methylene chloride solution was separated, the organic layer was concentrated and purified by silica gel chromatography to give the product 1.3g.
Ic: 1 H NMR (300 MHz, CDCl 3 ): [delta] 7.29 (m, 1H), 6.08 (m, 1H), 5.61 (m, 1H), 4.33-4.72 (m, 4H), 3.37-3.90 (m, 6H), 1.43-1.82 (m, 12H), 1.25 (s, 3H); ESI-MS m / z (M + 1) 427.
The solvent was removed, the residue was purified compound of Example 6 Ic (0.43g, 1mmol) was dissolved in 70% HF in pyridine was heated to 100 ~ 120 ℃, stirred for 5 hours, cooled, reduced pressure was purified through silica gel column to give a solid ( 0.18g, yield: 72%).
IIIa: 1 H NMR (300 MHz, DMSO-d 6 ): [delta] 11.48 (s, 1H), 7.82 (d, 1H, J = 6.0 Hz), 6.00 (d, 1H, J = 15.6 Hz), 5.67 (m , 2H), 5.30 (s, 1H), 3.85 (m, 3H), 3.62 (s, 1H), 1.25 (d, 3H, J = 16.8Hz), ESI-MS m / z (M-1) 259.
The compound of Example 6 Ic (50mg, 0.122mmol) was dissolved in methanol (1ml) was added 1N sodium hydroxide solution (0.2ml), stirred at room temperature overnight, water was added and the methylene chloride solution was separated, the organic layer was concentrated after purified by column chromatography to give the product (45mg, yield: 87%).
VA: 1 H NMR (300 MHz, CDCl 3 ): [delta] 7.89 (d, 1H, J = 4.5Hz), 6.01 (s, 1H), 5.95 (d, 1H, J = 4.5Hz), 5.65 (m, 2H ), 4.73 (m, 3H), 4.59 (m, 1H), 3.52-4.30 (m, 4H), 1.56-1.80 (m, 12H), 1.32 (s, 3H); ESI-MS m / z (M + 35) 461.
The mixture of Example 8 Compound Va (0.43g, 1mmol) was dissolved in dichloromethane and pyridine, was added DAST (0.32g), stirred for 24 hours, added dichloromethane (20ml) was diluted with water (30ml × 2) and washed , dried over anhydrous sodium sulfate, filtered, and concentrated under reduced pressure to obtain compound IIb. Compound IIb is dissolved in methanol (10ml) was added p-toluenesulfonic acid (200mg), stirred for 6 hours at room temperature, the methanol was removed under reduced pressure, silica gel column chromatography to give the product IIIa (180mg, yield: 75%).
IIIa: 1 H NMR (300 MHz, DMSO-d 6 ): [delta] 11.48 (s, 1H), 7.82 (d, 1H, J = 6.0 Hz), 6.00 (d, 1H, J = 15.6 Hz), 5.67 (m , 2H), 5.30 (s, 1H), 3.85 (m, 3H), 3.62 (s, 1H), 1.25 (d, 3H, J = 16.8Hz), ESI-MS m / z (M-1) 259.
The 2′-C- methyl uridine (0.2g, 0.8mmol) was dissolved in N, N- dimethylformamide (4ml) was added N, N’- carbonyldiimidazole (0.194g, 1.2mmol) and sodium bicarbonate (55mg, 0.66mmol), was heated to 130 ℃, stirred for 4 hours, cooled and the solvent was removed under reduced pressure, and the residue was dissolved in 70% HF in pyridine was heated to 140 ~ 150 ℃, stirred for 3 hours, cooled, The solvent was removed under reduced pressure, the residue was added to acetone and filtered to obtain a solid IIIa (0.12g, yield: 60%).
The 2′-C- methyl uridine (0.2g, 0.8mmol) was dissolved in N, N- dimethylformamide (4ml) was added diphenyl carbonate (0.256g, 1.2mmol) and sodium bicarbonate ( 55mg, 0.66mmol), was heated to 150 ℃, stirred for 6 hours, cooled and the solvent was removed under reduced pressure, and the residue was dissolved in 70% HF in pyridine was heated to 140 ~ 150 ℃, stirred for 3 hours, cooled and the solvent was removed under reduced pressure The residue was added to acetone and filtered to obtain a solid IIIa (0.13g, yield: 65%).
Under nitrogen, the compound of Example 9 Example Va (4.26g, 10mmol) was dissolved in dry tetrahydrofuran (100ml) was added triethylamine (6g, 60mmol), cooled to -78 ℃, was added trifluoromethanesulfonic anhydride (4.23g , 15mmol), stirred for 1 hour, the reaction system was added saturated ammonium chloride solution, extracted three times with methylene chloride, organic phases were combined, dried over anhydrous sodium sulfate, concentrated, and the residue was subjected to silica gel column chromatography to give the product Vb ( 4g, yield: 72%). ESI-MS m / z (M-1) 557.
Compound Vb (4g) was dissolved in dry tetrahydrofuran, was added tetrabutylammonium fluoride (1.87g, 7.1mmol), warmed to reflux, cooled to room temperature after heating for 1 hour, water was added to the reaction system, and extracted with methylene chloride three times, the combined organic phase was dried over anhydrous sodium sulfate, concentrated, and the residue was subjected to silica gel column chromatography to give the product IIb (2.7g, yield: 88%). ESI-MS m / z (M-1) 427.
Compound IIb (2.7g) was dissolved in methanol (20ml) was added 3M hydrochloric acid (10ml), 50 ℃ stirred for 8 hours, and concentrated to give a solid, was added acetonitrile, beating, and filtered to give the product IIIa (1g, yield: 61%).
IIIa: 1 H NMR (300 MHz, DMSO-d 6 ): [delta] 11.48 (s, 1H), 7.82 (d, 1H, J = 6.0 Hz), 6.00 (d, 1H, J = 15.6 Hz), 5.67 (m , 2H), 5.30 (s, 1H), 3.85 (m, 3H), 3.62 (s, 1H), 1.25 (d, 3H, J = 16.8Hz), ESI-MS m / z (M-1) 259.
UPDATE DEC2015……….

SOFOSBUVIR
NEW PATENT WO2015188782,
(WO2015188782) METHOD FOR PREPARING SOFOSBUVIR
CHIA TAI TIANQING PHARMACEUTICAL GROUP CO., LTD [CN/CN]; No. 8 Julong North Rd., Xinpu District Lianyungang, Jiangsu 222006 (CN)

![]()
Sofosbuvir synthesis routes currently used include the following two methods:

https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2015188782&redirectedID=true

Preparation Example 1 sofosbuvir implementation
At 0 ℃, dichloro-phenyl phosphate (6.0g, 28.4mmol) in dry dichloromethane (30ml) and stirred added alanine isopropyl ester hydrochloride (4.8g, 28.4mmol), the mixture After stirring and cooling to -55 ℃, was slowly added dropwise triethylamine (6.5g, 64mmol) and dichloromethane (30ml) mixed solution, keeping the temperature during at -55 ℃, dropping was completed, stirring was continued for 60 minutes, after liters to -5 ℃ stirred for 2 hours, TLC monitored the reaction was complete. To remove triethylamine hydrochloride was filtered and the filtrate evaporated under reduced pressure to give compound 3-1 as a colorless oil (Sp / Rp = 1/1).
31 PNMR (CDCl 3 , 300 Hz, H 3 PO 4 as internal standard): δ8.25 & 7.94 (1: 1);
1 HNMR (CDCl 3 , 300 MHz): δ7.39-7.34 (m, 2H), 7.27-7.18 (m, 3H), 5.10-5.02 (m, 1H), 4.51 (br, 1H), 4.11 (m, 1H ), 1.49 (d, 3H), 1.29-1.24 (m, 6H);
13 C NMR (CDCl 3 , 300 MHz): δ172.1 (Rp), 196.3 (Sp), 129.8,129.6 (d), 125.9,120.5 (d), 69.7 (d), 50.7 (d), 21.6 (d), 20.4 (d).
At 5 ℃, the compound of formula 2 (5.20g, 20.0mmol) in dry THF (30ml) and stirred at t-butyl chloride (1.0M THF solution, 42ml, 42.0mmol). The reaction temperature was raised to 25 ℃, and the mixture was stirred for 30 minutes. After addition of lithium chloride (21.0mmol), was slowly added dropwise the compound 3-1 (approximately 28.4mmol) and THF (30ml) mixed solution, keeping the temperature during at 5 ℃. Bi drops, stirred for 15 hours. With aqueous 1N HCl (25ml) The reaction solution was quenched (HPLC assay Sp: Rp ratio of 4: 1). Toluene was added (100ml), temperature was raised to room temperature. The organic layer was washed with 1N HCl, water, 5% Na 2 CO 3 and washed with brine, dried over anhydrous magnesium sulfate, filtered, and the solvent was distilled off under reduced pressure to a solid, was added methylene chloride (20ml), stirred for 5 minutes plus isopropyl ether, stirring was continued for 2 hours, the precipitated solid was filtered off. The solid was dissolved by heating in dichloromethane (60ml), slowly cooled to room temperature and the precipitated crystalline solid. Repeat if necessary obtain pure crystalline sofosbuvir (2.6g, yield 25%, HPLC purity measured 98.8%).
31 PNMR (CDCl 3 , 300 Hz, H 3 PO 4 as internal standard): δ3.54ppm;
13 C NMR (CDCl 3 , 300 Hz): δ173.1 (d), 162.7 (s), 150.2 (d), 139.3 (d), 129.6 (q);
Preparation of compounds of formula 2 shown in Example 3-2
(1) a nucleophilic reagent as NaSCN, the phase transfer catalyst is TBAB
The compound (product of Example 1, step (a)) is represented by the formula 3-1 is dissolved in dichloromethane (20ml) was added TBAB (2.8mmol), the NaSCN (35mmol) in water (2.0ml) was added dropwise It was added to the reaction solution. Dropping was completed, stirring was continued for 60 minutes, the solid was removed by filtration. The filtrate was washed with water, add MgSO 4 dried for 24 hours. Filtered, and the filtrate was evaporated under reduced pressure, to obtain a compound of formula 3-2 as (where X = SCN).
1 HNMR (CDCl 3 , 500Hz): δ7.32-7.13 (m, 3H), 7.08-7.02 (m, 2H), 5.0-4.9 (m, 1H), 3.92 (m, 1H), 1.49 (m, 3H ), 1.23-1.17 (m, 6H);
31 PNMR (CDCl 3 , 300 Hz, H 3 PO 4 internal standard): δ-18.16 / -18.26.
(2) nucleophile NaSCN, phase transfer catalyst is 18-crown-6 ether
The compound (product of Example 1, step (a)) is represented by the formula 3-1 is dissolved in ethyl acetate (20ml) was added 18-crown -6 (2.8mmol), the NaSCN (35mmol) was added to the above the reaction mixture. Dropping was completed, stirring was continued for 60 minutes, the solid was removed by filtration. The filtrate was washed with water, add MgSO 4 dried for 24 hours. Filtered, and the filtrate was evaporated under reduced pressure, to obtain a compound of formula 3-2 as (where X = SCN).
(3) nucleophile NaSCN, phase transfer catalyst is TBAB and 18-crown-6
The compound (product of Example 1, step (a)) is represented by the formula 3-1 is dissolved in dichloromethane (20ml) was added TBAB (2.8mmol) and 18-crown -6 (2.8mmol), the NaSCN (35mmol) in water (2.0ml) was added to the reaction solution. Dropping was completed, stirring was continued for 60 minutes, the solid was removed by filtration. The filtrate was washed with water, add MgSO 4 dried for 24 hours. Filtered, and the filtrate was evaporated under reduced pressure, to obtain a compound of formula 3-2 as (where X = SCN).
(4) nucleophile as NaN 3 , phase transfer catalyst is TBAB
The compound (product of Example 1, step (a)) is represented by the formula 3-1 is dissolved in dichloromethane (20ml) was added TBAB (2.8mmol), the NaN 3 (35 mmol) in water (2.0ml) solution of was added dropwise to the reaction solution. Dropping was completed, stirring was continued for 60 minutes, the solid was removed by filtration. The filtrate was washed with water, add MgSO 4 dried for 24 hours. Filtered, and the filtrate was evaporated under reduced pressure, to obtain a compound of formula 3-2 as (where X = N 3 ).
1 HNMR (CDCl 3 , 500Hz): δ7.30-7.33 (m, 2H), 7.27-7.21 (m, 3H), 5.10-5.05 (m, 1H), 4.12-4.00 (m, 1H), 1.43 (d , 3H), 1.28-1.17 (m, 6H);
31 PNMR- (CDCl 3 , 300 Hz, H 3 PO 4 internal standard): δ2.04 / 2.19.
(5) the nucleophilic reagent is KCN, the phase transfer catalyst is TBAB
The compound was dissolved in methylene chloride as in formula 3-1 (20ml), was added TBAB (2.8mmol), the KCN (35mmol) in water (2.0ml) was added dropwise to the reaction solution. Dropping was completed, stirring was continued for 60 minutes, the solid was removed by filtration. The filtrate was washed with water, add MgSO 4 dried for 24 hours. Filtered, and the filtrate was evaporated under reduced pressure to remove the solvent to give a compound as shown in Formula 3-2 (where X = CN).
1 HNMR (CDCl 3 , 300 Hz): δ7.22-7.13 (m, 3H), 7.09-7.02 (m, 2H), 5.01-4.95 (m, 1H), 4.08-3.93 (m, 1H), 1.43-1.35 (m, 3H), 1.20-1.17 (m, 6H);
31 PNMR (CDCl 3 , 300 Hz, H 3 PO 4 internal standard): δ-2.71 / -2.93.
Preparation Example 3 sofosbuvir implementation
Under 5 ℃, the compound (5.20g, 20.0mmol) as shown in Equation 2 in dry THF (30ml) in. T-butyl chloride was added with stirring (1.0M THF solution, 42ml, 42.0mmol). The reaction temperature was raised to 25 ℃, and the mixture was stirred for 30 minutes. After addition of lithium chloride (21.0mmol), was slowly added dropwise a compound of formula 3-2 (Preparation Example 2 28.4 mmol, obtained) and THF (30ml) mixed solution, keeping the temperature during at 5 ℃. After dropping was completed, the mixture was stirred for 15 hours. With aqueous 1N HCl (25ml) The reaction solution was quenched (HPLC assay Sp: Rp ratio of 6: 1). After further addition of toluene (100ml), temperature was raised to room temperature. The organic layer was washed with 1N HCl, water, 5% Na 2 CO 3 and washed with brine, dried over anhydrous magnesium sulfate, filtered, and the solvent was distilled off under reduced pressure to a solid, was added methylene chloride (20ml), stirred for 5 minutes plus isopropyl ether, stirring was continued for 2 hours, the precipitated solid was filtered off. The solid was dissolved by heating in dichloromethane (60ml), slowly cooled to room temperature and the precipitated crystalline solid. Repeat if necessary obtain pure crystalline sofosbuvir (3.6g, yield 34%, HPLC purity measured 98.7%).
1 HNMR (CDCl 3 , 300 MHz): [delta] 8.63 (s, 1H, NH), 7.46 (d, 1H, C6-H), 7.36 (t, 2H, O-aromatic), 7.18-7.24 (m, 3H, m, P-aromatic), 6.20-6.14 (d, 1H, Cl’-H), 5.70-5.68 (d, 1H, C5-H), 5.05-4.97 (m, 1H, CH- (CH 3 ) 2 ) , 4.57-4.41 (m, 2H, C5′-H2), 4.12-4.09 (d, 1H, C3′-H), 4.06-3.79 (m, 3H, C3′-OH, C4′-H, Ala-CH -CH 3 ), 3.79 (s, 1H, Ala-NH), 1.44 (d, 3H, C2′-H3), 1.36-1.34 (d, 3H, Ala-CH 3 ), 1.25-1.23 (t, 6H, CH- (CH 3 ) 2 );
P 31 NMR (CDCl 3 , 300 Hz, H 3 PO 4 internal standard): δ3.56.
Under 5 ℃, the compound (5.20g, 20.0mmol) as shown in Equation 2 in dry THF (30ml) in. T-butyl chloride was added with stirring (1.0M THF solution, 42ml, 42.0mmol). The reaction temperature was raised to 25 ℃, and the mixture was stirred for 30 minutes. Was added lithium chloride (21.0mmol), was slowly added dropwise after the compound of formula 3-2 obtained in Preparation Example 2 (about 28.4 mmol) and THF (30ml) mixed solution, keeping the temperature during at 5 ℃. Bi drops, stirred for 15 hours. With aqueous 1N HCl (25ml) The reaction solution was quenched (HPLC assay Sp: Rp ratio of 7: 1). After further addition of toluene (100ml), temperature was raised to room temperature. The organic layer was washed with 1N HCl, water, 5% Na 2 CO 3 and washed with brine, dried over anhydrous magnesium sulfate, filtered, and the solvent was distilled off under reduced pressure to a solid, was added methylene chloride (20ml), stirred for 5 minutes plus isopropyl ether, stirring was continued for 2 hours, the precipitated solid was filtered off. The solid was dissolved by heating in dichloromethane (60ml), slowly cooled to room temperature and the precipitated crystalline solid. Repeat if necessary obtain pure crystalline sofosbuvir (4.2g, yield 40%, HPLC purity measured 98.8%).
1 HNMR (CDCl 3 , 300 MHz): [delta] 8.63 (s, 1H, NH), 7.46 (d, 1H, C6-H), 7.36 (t, 2H, O-aromatic), 7.18-7.24 (m, 3H, m, P-aromatic), 6.20-6.14 (d, 1H, Cl’-H), 5.70-5.68 (d, 1H, C5-H), 5.05-4.97 (m, 1H, CH- (CH 3 ) 2 ) , 4.57-4.41 (m, 2H, C5′-H2), 4.12-4.09 (d, 1H, C3′-H), 4.06-3.79 (m, 3H, C3′-OH, C4′-H, Ala-CH -CH 3 ), 3.79 (s, 1H, Ala-NH), 1.44 (d, 3H, C2′-H3), 1.36-1.34 (d, 3H, Ala-CH 3 ), 1.25-1.23 (t, 6H, CH- (CH 3 ) 2 );
P 31 NMR (CDCl 3 , 300 Hz, H 3 PO 4 internal standard): δ3.56.
Under 5 ℃, the compound (5.20g, 20.0mmol) as shown in Equation 2 in dry THF (30ml) in. T-butyl chloride was added with stirring (1.0M THF solution, 42ml, 42.0mmol). The reaction temperature was raised to 25 ℃, and the mixture was stirred for 30 minutes. After addition of lithium chloride (21.0mmol), was slowly added dropwise a compound of formula 3-2 obtained in Preparation Example 2 (about 28.4 mmol) and THF (30ml) mixed solution, keeping the temperature during at 5 ℃. Bi drops, stirred for 15 hours. With aqueous 1N HCl (25ml) The reaction solution was quenched (HPLC assay Sp: Rp ratio of 6: 1). After further addition of toluene (100ml), temperature was raised to room temperature. The organic layer was washed with 1N HCl, water, 5% Na 2 CO 3 and washed with brine, dried over anhydrous magnesium sulfate, filtered, and the solvent was distilled off under reduced pressure to a solid, was added methylene chloride (20ml), stirred for 5 minutes plus isopropyl ether, stirring was continued for 2 hours, the precipitated solid was filtered off. The solid was dissolved by heating in dichloromethane (60ml), slowly cooled to room temperature and the precipitated crystalline solid. Repeat if necessary obtain pure crystalline sofosbuvir (4.02g, yield 40%, HPLC purity measured 98.8%).
1 HNMR (CDCl 3 , 300 MHz): [delta] 8.63 (s, 1H, NH), 7.46 (d, 1H, C6-H), 7.36 (t, 2H, O-aromatic), 7.18-7.24 (m, 3H, m, P-aromatic), 6.20-6.14 (d, 1H, Cl’-H), 5.70-5.68 (d, 1H, C5-H), 5.05-4.97 (m, 1H, CH- (CH 3 ) 2 ) , 4.57-4.41 (m, 2H, C5′-H2), 4.12-4.09 (d, 1H, C3′-H), 4.06-3.79 (m, 3H, C3′-OH, C4′-H, Ala-CH -CH 3 ), 3.79 (s, 1H, Ala-NH), 1.44 (d, 3H, C2′-H3), 1.36-1.34 (d, 3H, Ala-CH 3 ), 1.25-1.23 (t, 6H, CH- (CH 3 ) 2 );
P 31 NMR (CDCl 3 , 300 Hz, H 3 PO 4 internal standard): δ3.56.




















































 Cod liver oil has been a popular supplement for many years and naturally contains very high levels of vitamin A and vitamin D. Cod liver oil provides 10001IU (1667% DV) per 100 gram serving, or 1360IU (340% DV) in a single tablespoon.
Cod liver oil has been a popular supplement for many years and naturally contains very high levels of vitamin A and vitamin D. Cod liver oil provides 10001IU (1667% DV) per 100 gram serving, or 1360IU (340% DV) in a single tablespoon. Various types of fish are high in vitamin D. Typically raw fish contains more vitamin D than cooked, and fatty cuts will contain more than lean cuts. Further, fish canned in oil will have more vitamin D than those canned in water. Raw fish is typically eaten in the form of sushi. Raw Atlantic Herring provides the most vitamin D with 1628IU (271% DV) per 100 gram serving, 2996IU (499% DV) per fillet, and 456IU (76% DV) per ounce. It is followed by Pickled Herring with 680IU (113% DV) per 100g serving, Canned Salmon (127% DV), Raw Mackerel (60% DV), Oil Packed Sardines (45% DV), Canned Mackerel (42% DV), and oil packed Tuna (39% DV).
Various types of fish are high in vitamin D. Typically raw fish contains more vitamin D than cooked, and fatty cuts will contain more than lean cuts. Further, fish canned in oil will have more vitamin D than those canned in water. Raw fish is typically eaten in the form of sushi. Raw Atlantic Herring provides the most vitamin D with 1628IU (271% DV) per 100 gram serving, 2996IU (499% DV) per fillet, and 456IU (76% DV) per ounce. It is followed by Pickled Herring with 680IU (113% DV) per 100g serving, Canned Salmon (127% DV), Raw Mackerel (60% DV), Oil Packed Sardines (45% DV), Canned Mackerel (42% DV), and oil packed Tuna (39% DV). A breakfast staple in the Americas, most commercial cereals are fortified with the essential vitamins and nutrients. Exercise caution and check food labels when purchasing cereals, be sure to pick products that have little or no refined sugars, and no partially hydrogenated oils! Fortified cereals can provide up to 342IU (57% DV) per 100 gram serving (~2 cups), and even more if combined with fortified dairy products or fortified soy milk. Products vary widely so be sure to check the nutrition label before buying.
A breakfast staple in the Americas, most commercial cereals are fortified with the essential vitamins and nutrients. Exercise caution and check food labels when purchasing cereals, be sure to pick products that have little or no refined sugars, and no partially hydrogenated oils! Fortified cereals can provide up to 342IU (57% DV) per 100 gram serving (~2 cups), and even more if combined with fortified dairy products or fortified soy milk. Products vary widely so be sure to check the nutrition label before buying. In addition to vitamin D, Oysters are a great source of vitamin b12, zinc, iron, manganese, selenium, and copper. Oysters are also high in cholesterol and should be eaten in moderation by people at risk of heart disease or stroke. Raw wild caught Eastern Oysters provide 320IU (80% DV) per 100 gram serving, 269IU (67% DV) in six medium oysters.
In addition to vitamin D, Oysters are a great source of vitamin b12, zinc, iron, manganese, selenium, and copper. Oysters are also high in cholesterol and should be eaten in moderation by people at risk of heart disease or stroke. Raw wild caught Eastern Oysters provide 320IU (80% DV) per 100 gram serving, 269IU (67% DV) in six medium oysters. Caviar is a common ingredient in sushi and more affordable than people think. Caviar provides 232IU (58% DV) of vitamin D per 100 gram serving, or 37.1IU (9% DV) per teaspoon.
Caviar is a common ingredient in sushi and more affordable than people think. Caviar provides 232IU (58% DV) of vitamin D per 100 gram serving, or 37.1IU (9% DV) per teaspoon. Fortified soy products are often fortified with both vitamin D and calcium. Fortified Tofu can provide up to 157IU (39% DV) of vitamin D per 100 gram serving, or 44IU (11% DV) per ounce. Fortified Soy Milk can provide up to 49IU (12% DV) of vitamin D per 100 gram serving, 119IU (30% DV) per cup. Amounts of vitamin D vary widely between products, so be sure to check nutrition facts for vitamin D content.
Fortified soy products are often fortified with both vitamin D and calcium. Fortified Tofu can provide up to 157IU (39% DV) of vitamin D per 100 gram serving, or 44IU (11% DV) per ounce. Fortified Soy Milk can provide up to 49IU (12% DV) of vitamin D per 100 gram serving, 119IU (30% DV) per cup. Amounts of vitamin D vary widely between products, so be sure to check nutrition facts for vitamin D content. Salami, Ham, and Sausages are a good source of vitamin b12, and copper. Unfortunately, they are also high in cholesterol and sodium, and so should be limited by people at risk of hypertension, heart attack, and stroke. Salami provides 62.0IU (16% DV) of vitamin D per 100 gram serving, or 16.7IU (4% DV) per ounce (3 slices). It is followed by Bologna Pork 56IU (9% DV) per 100 grams, and Bratwurst 44IU (7% DV) per 100 gram serving.
Salami, Ham, and Sausages are a good source of vitamin b12, and copper. Unfortunately, they are also high in cholesterol and sodium, and so should be limited by people at risk of hypertension, heart attack, and stroke. Salami provides 62.0IU (16% DV) of vitamin D per 100 gram serving, or 16.7IU (4% DV) per ounce (3 slices). It is followed by Bologna Pork 56IU (9% DV) per 100 grams, and Bratwurst 44IU (7% DV) per 100 gram serving. Dairy products are already high in calcium, so it makes sense to fortify them with vitamin D. Milk can provide up to 52.0IU (13% DV) of vitamin D per 100 gram serving, 127IU (32% DV) per cup. Cheese can provide up to 6.6IU (2% DV) in a cubic inch, and butter provides 7.8IU (2% DV) in a single tablespoon. Check nutrition labels for exact amounts.
Dairy products are already high in calcium, so it makes sense to fortify them with vitamin D. Milk can provide up to 52.0IU (13% DV) of vitamin D per 100 gram serving, 127IU (32% DV) per cup. Cheese can provide up to 6.6IU (2% DV) in a cubic inch, and butter provides 7.8IU (2% DV) in a single tablespoon. Check nutrition labels for exact amounts. In addition to vitamin D, eggs are a good source of vitamin B12, and protein. Eggs provide 37.0IU (9% DV) of vitamin D per 100 gram serving, or 17.0IU (4% DV) in a large fried egg.
In addition to vitamin D, eggs are a good source of vitamin B12, and protein. Eggs provide 37.0IU (9% DV) of vitamin D per 100 gram serving, or 17.0IU (4% DV) in a large fried egg. More than just a high vitamin D food, mushrooms also provide Vitamin B5 (Pantothenic Acid) and copper. Lightly cooked white button mushrooms provide the most vitamin D with 27.0IU (7% DV) per 100 gram serving, or 7.6IU (2% DV) per ounce.
More than just a high vitamin D food, mushrooms also provide Vitamin B5 (Pantothenic Acid) and copper. Lightly cooked white button mushrooms provide the most vitamin D with 27.0IU (7% DV) per 100 gram serving, or 7.6IU (2% DV) per ounce.